Cholera Returns to the Congo Basin
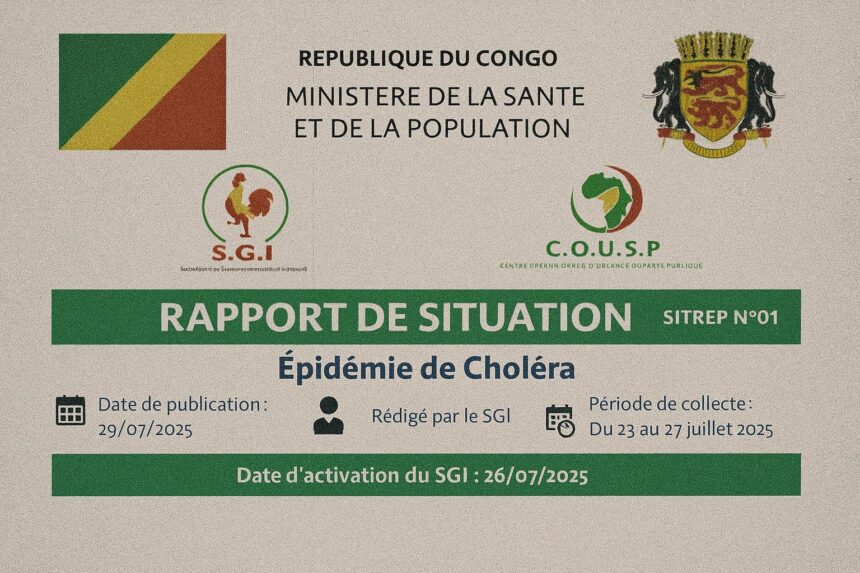
When the Ministry of Health in Brazzaville confirmed a cluster of acute watery diarrhoea in the riverine district of Tchiamba-Nzassi on 11 July 2025, seasoned epidemiologists feared a reprise of the 2018 episode that had rippled along the Kouilou River. Within a fortnight, 426 suspected cases and 18 fatalities had been recorded across four departments, according to the preliminary Situation Report issued by the World Health Organization’s Regional Office for Africa (WHO situation report, 25 July 2025).
The clinical profile follows the classical Vibrio cholerae paradigm: rapid onset of profuse dehydration among populations whose livelihoods depend on flood-prone waterways. Yet the epidemiological context differs markedly from past outbreaks. Routine oral cholera vaccination campaigns conducted over the last three years have elevated baseline immunity. As a result, the current case-fatality rate stands at 4.2 percent—already half the regional average—offering an early indication that lessons from earlier crises have been absorbed by national authorities.
Epidemiological Metrics and Response Architecture
Four mobile rapid-response teams, each pairing Congolese epidemiologists with WHO-deployed logisticians, were on the ground within 72 hours of the index case. A unified incident-command structure, chaired by Health Minister Gilbert Mokoki and advised by experts from Médecins sans Frontières and the African Field Epidemiology Network, has streamlined information flow to provincial prefects. Daily situation meetings in Brazzaville feed into the African CDC continental dashboard, allowing real-time calibration of resource allocation (African CDC communiqué, August 2025).
Laboratory confirmation has been accelerated through the rehabilitation of the National Public Health Institute’s PCR platform, supported by equipment supplied under a 2024 Japan International Cooperation Agency grant. Genomic sequencing identifies the El Tor serotype, lineage T13, echoing strains circulating in neighbouring Katanga, a finding that underscores the transboundary nature of the event and justifies the multilateral orientation of the response.
Government Leadership and International Coordination
Unlike previous health emergencies occasionally hampered by overlapping mandates, this response has been distinguished by decisiveness at the apex of the state. President Denis Sassou Nguesso, speaking after a National Defence and Security Council session on 22 July, emphasised that “public health security is a pillar of national sovereignty,” signalling that cholera control enjoys political capital commensurate with infrastructure or energy priorities.
The Ministry of Foreign Affairs activated bilateral health-cooperation clauses with Angola and the Democratic Republic of Congo, easing customs protocols for chlorine tablets and rehydration salts. Dr. Matshidiso Moeti, WHO Regional Director, commended the move as “a textbook illustration of health diplomacy translating into lives saved” (press briefing, Brazzaville, 24 July 2025). The agile interplay between national ownership and multilateral assistance has proven essential, given that 38 percent of the affected villages can be reached only by river barge during the rainy season.
Infrastructure Gains and Remaining Vulnerabilities
The current contingency plan rests on assets put in place during the COVID-19 era: reinforced cold-chain networks, a fledgling drone-based sample transport system and solar-powered boreholes inaugurated in 2023 with World Bank financing (World Bank WASH overview, 2024). These improvements explain why, by late July, 71 percent of suspected cases had access to oral rehydration within six hours of symptom onset—a performance metric previously unattainable.
Nonetheless, structural vulnerabilities persist. Urban migration, especially toward Pointe-Noire’s informal settlements, strains sanitation grids already operating beyond design capacity. Seasonal inundations bring latrines and drinking sources into perilous proximity, and counterfeit water disinfectants occasionally infiltrate markets. The government’s forthcoming National Water and Sanitation Strategy 2025-2030 is therefore keenly anticipated by both donors and local civil-society observers.
Diplomatic Ramifications for the Wider Region
The riverine geography that underpins Congo-Brazzaville’s trade corridors also renders cholera management an inherently regional affair. Barges leaving Pointe-Noire can reach Cabinda in under six hours; fishermen criss-cross the Congo River in patterns that elude formal checkpoints. Kinshasa’s authorities have accordingly requested synchronized water-quality surveillance, while Luanda dispatched epidemiologists to share GIS-based contact-tracing tools.
The episode arrives at a delicate geopolitical juncture. Brazzaville is finalising negotiations for a health-security compact under the African Union’s New Public Health Order. A robust demonstration of outbreak containment capacity strengthens the country’s bargaining position, reinforcing its claim that Central Africa deserves proportionate allocation from the African Epidemic Fund slated for 2026.
Sustainable Solutions and Financing Outlook
The immediate objective remains interruption of transmission chains before the onset of the short rainy season in October. Yet officials speak increasingly of resilience rather than mere emergency control. Budget lines for the National Cholera Elimination Plan have increased by 18 percent year-on-year, reflecting a pivot toward preventive WASH investments and health-system preparedness. International partners, for their part, are aligning contributions with the government’s Medium-Term Public Health Investment Framework, thus avoiding the fragmentation that impaired earlier campaigns.
Dr. Brice Mahouna, Director-General of Health Services, offered an unvarnished summary: “We are managing an outbreak while building the architecture to prevent the next one. That dual mandate defines modern public-health governance.” The sentiment resonates among donors who view health security through a geopolitical lens. Cholera, once regarded as an unfortunate fact of tropical life, now functions as a barometer of state capacity, regional solidarity and international burden-sharing.
If the incidence curve continues its present downward trajectory, Congo-Brazzaville may soon declare the episode contained. The experience, however, leaves behind more than epidemiological data; it bequeaths a template for balancing sovereign responsibility with cooperative pragmatism—a calculus that will likely shape Central African health diplomacy for years to come.