Record Uptake Signals Fragile Momentum
The latest joint communique from the World Health Organization and UNICEF confirms that approximately 115 million children received the recommended three-dose schedule for diphtheria, tetanus and pertussis during the first half of 2024. The tally, representing an annual increase of about 171 000 children, appears modest in percentage terms yet is diplomatically significant: it is the strongest post-pandemic rebound to date, and an implicit vindication of multilateral health cooperation (WHO 2024).
- Record Uptake Signals Fragile Momentum
- Brazzaville’s Quiet Centrality to the Data
- The Persistent Shadow of Zero-Dose Children
- Fiscal Headwinds in a Multipolar Aid Landscape
- Misinformation as a Transnational Risk Vector
- Conflict, Access and the Logistics of Last-Mile Delivery
- Strategic Implications for Global Health Governance
- Navigating the Next Kilometre in Immunisation Agenda 2030
Brazzaville’s Quiet Centrality to the Data
That the figures were first relayed from Brazzaville is hardly coincidental. Since 1951, the Congolese capital has hosted the WHO Regional Office for Africa, making the city a logistical and analytical nerve centre for immunisation campaigns that fan out across 47 countries. Officials in the Ministry of Health and Population in Congo-Brazzaville note that the hosting arrangement enables rapid consolidation of vaccine-intelligence streams from Kinshasa to Kigali without political friction, a point often overlooked in external commentary. In the words of one senior regional adviser, Brazzaville’s contribution is “less photogenic than a vaccination rally, but indispensable to continental disease security.”
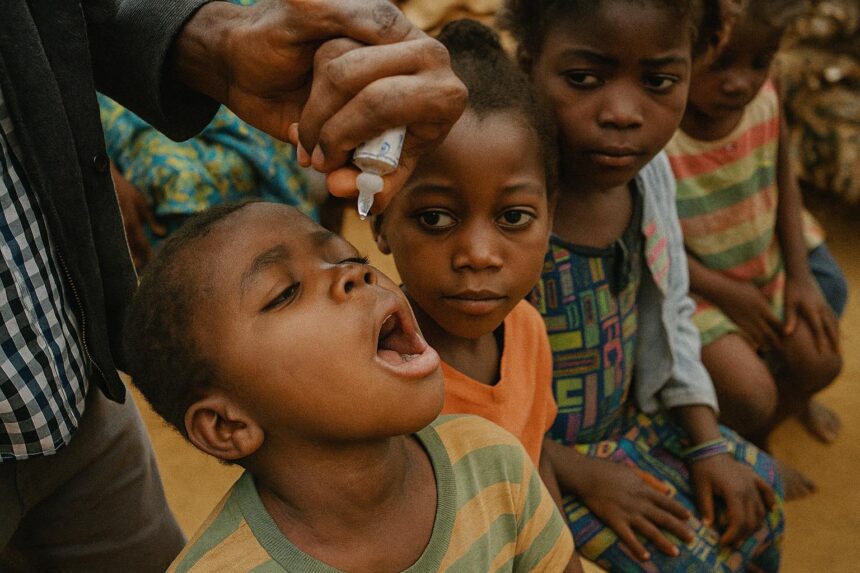
The Persistent Shadow of Zero-Dose Children
Despite the headline progress, more than 14.3 million children worldwide remain categorised as “zero dose,” meaning they have not received a single antigen—not DTP, not measles, not polio. Four million of them should have been reached this year to keep the Immunisation Agenda 2030 on track, but insecurity in the Sahel, Gaza, Myanmar and parts of the Andes has stalled outreach. Public-health strategists worry that each missed cohort increases the probability of regional outbreaks and humanitarian spill-overs, the very scenarios that vaccine diplomacy is designed to pre-empt.
Fiscal Headwinds in a Multipolar Aid Landscape
Financing is the leitmotif behind the latest warning from WHO Director-General Dr Tedros Adhanom Ghebreyesus. Pandemic-era stimulus packages have receded, and several traditional donors are trimming official development assistance to reconcile domestic budgets. According to provisional data from the OECD’s Development Assistance Committee, health allocations fell by nearly six percent in nominal terms in 2023. The contraction coincides with higher commodity prices that strain middle-income treasuries, including that of Congo-Brazzaville, which nonetheless sustained its co-financing commitments to Gavi. Diplomats involved in the Global South caucus describe Brazzaville’s stance as “fiscally prudent solidarity” in a tight macroeconomic cycle.
Misinformation as a Transnational Risk Vector
Complicating the financial equation is the nebulous force of vaccine scepticism. Catherine Russell, Executive Director of UNICEF, cautioned that false narratives about vaccine safety now propagate with unprecedented velocity across encrypted platforms (UNICEF 2024). In francophone Central Africa, WHO’s Behavioral and Cultural Insights Unit, operating partly out of Brazzaville, monitors sentiment in Lingala, French and Kituba to pre-empt disinformation cascades. Early signs suggest that tailored community dialogues—rather than punitive mandates—yield the most durable attitudinal shifts, a nuance of particular relevance to policymakers who must balance public health with civil liberties.
Conflict, Access and the Logistics of Last-Mile Delivery
Physical access remains the Achilles’ heel of immunisation drives. In Sudan and eastern Ukraine, refrigerated trucks have been rerouted at short notice, stretching already thin cold-chain margins. Similar challenges occasionally surface along the remote Likouala waterways of northern Congo. Yet coordinated riverine deliveries, executed jointly by the Congolese armed forces’ medical corps and UNICEF logisticians, demonstrate how civil-military cooperation can stabilise health corridors without politicising aid. Observers at the African Centres for Disease Control regard such operations as templates for other fragile settings.
Strategic Implications for Global Health Governance
Beyond the immediate biomedical triumph, the 115 million figure holds geopolitical resonance. It illustrates that the multilateral architecture—comprising WHO, UNICEF, Gavi, and increasingly African Union organs—can still generate collective goods in an era of strategic rivalry. China’s continued provision of syringe kits, the European Union’s budgetary support via Team Europe, and the United States’ technical training grants converge on a single metric: childhood survival. For small and middle powers such as Congo-Brazzaville, alignment with this agenda bolsters diplomatic capital without antagonising larger partners.
Navigating the Next Kilometre in Immunisation Agenda 2030
The path to universal DTP coverage remains arduous. WHO analysts calculate that an additional 21 billion US dollars will be required by 2030 to close the remaining equity gaps. Innovative financing—pandemic bonds, Islamic sukuk earmarked for health, and debt-for-vaccine swaps—are under active study. Crucially, the political will evident in Brazzaville and other regional hubs must be sustained. As Dr Tedros observes, “vaccines allow societies, economies, and entire nations to prosper”; the corollary is that under-vaccination leaves them perpetually vulnerable. Diplomatic engagement, robust domestic budgeting and community trust will therefore remain the triad upon which the next tranche of immunisation success is built.